Improving Management of Rapidly Deteriorating Pediatric Patients
Response to deteriorating patients is critically important for patient safety and a significant marker of quality of care. Professional efforts to improve this response have focused on the recognition of patient deterioration (afferent limb) and the subsequent escalation of care, often involving Medical Emergency Teams (MET defferent limb).
Case Study Details
- 35% Reduction in length of stay in PICU
- 71% Reduction in mortalities in PICU
- 334 PICU bed days saved
- ability to treat an additional 52 patients in the PICU per year
- Cost savings: ₤801,600
- Annual ROI 10.8x
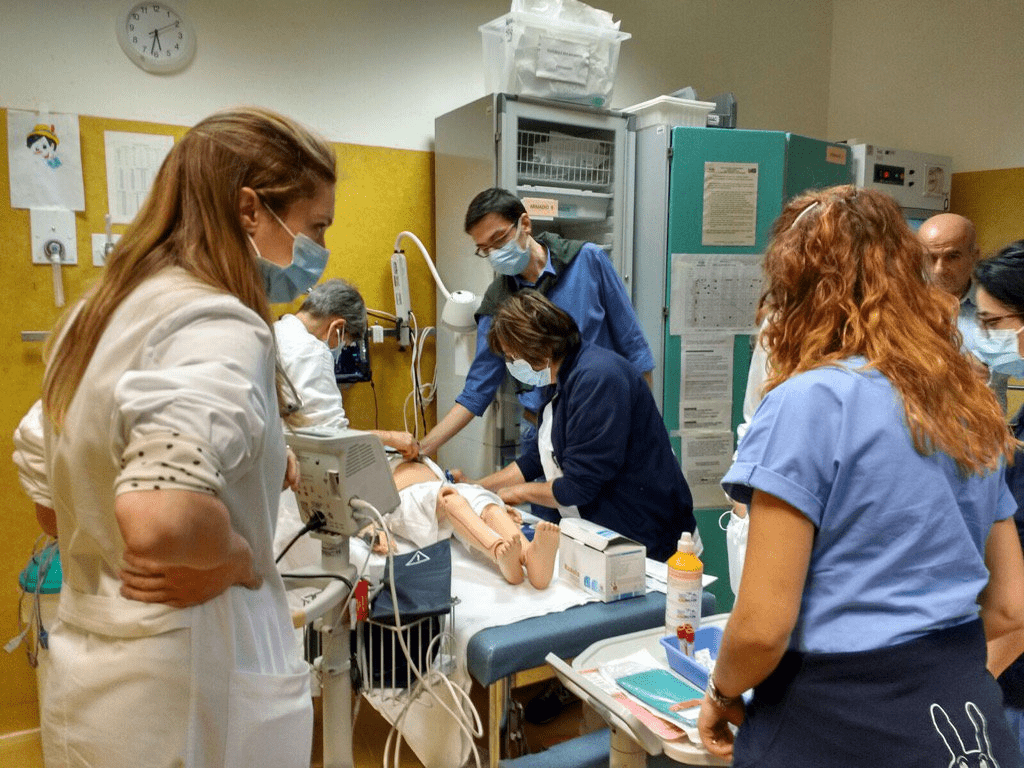
Weekly InSitu training – Teams trained in groups of 6 in their clinical roles focused on the following:
- recognition of deteriorating child
- role recognition
- communication within team
- early involvement of senior staff
- early communication with pediatric intensive care
- ₤74,250 per annum
- ₤46,800 Staff Training
- ₤17,450 Protected Training Time
- ₤10,000 Consumables/Simulator
Ongoing (2 hrs weekly training)
- 2 Trainers, 1 consultant, 1 senior nurse
- mid fidelity pediatric simulator and mid fidelity infant simulator
- properly trained staff to support training initiative
- learner time to train away from clinical duties
- typical length of stay 9.9 days
- patient mortality rate 7/56 admissions
- Higher Mortality Rate
- Less than optimal management of deteriorating patients
- reduced capacity by 52 patients due to inefficiencies
Decision Maker Talking Points
- 71% Reduction in mortalities in PICU
- 35% Reduction in length of stay in PICU
- Be able to treat an additional 52 patients per year in the PICU
- Better patient care for community, be able to serve more people with same resources
- Savings of ₤801,600 in unnecessary expenses
- Savings of ₤801,600 in unnecessary expenses
- 35% Reduction in length of stay in PICU
- Be able to treat an additional 52 patients per year in the PICU
- Annual ROI 10.8x
- 71% Reduction in mortalities in PICU
- 35% Reduction in length of stay in PICU
- Be able to treat an additional 52 patients per year in the PICU
- 334 PICU bed days saved
- need to train medical students with evidence based best practices
- need to have medical students training in an IPE environment to best prepare for current needs in Hospitals
- have students prepared to operate in high risk, time pressured critical environments
- better preparing the medical students given limitations on clinical hours
- practicing in a simulated environment instead of on actual patients
- need to train nursing students with evidence based best practices
- need to have nursing students training in an IPE environment to best prepare for current needs in Hospitals
- better preparing the nursing students given limitations access to clinical placements
- practicing in a simulated environment instead of on actual patients
- Better efficiency in the care of patients with the most common problems
- increase the ability of staff to treat more patients
- ability to retain staffing by showing value for patient satisfaction
- ability to better adjust behavior as teams train together
- making the case will involve a fully engaged staff of passionate educators
- make clear that faculty educators must be trained to conduct deliberate practice and feedback
- support a part of the institutions patient safey initiative to align with mission focus
- focus on capturing the appropriate ROI metrics for you environment
