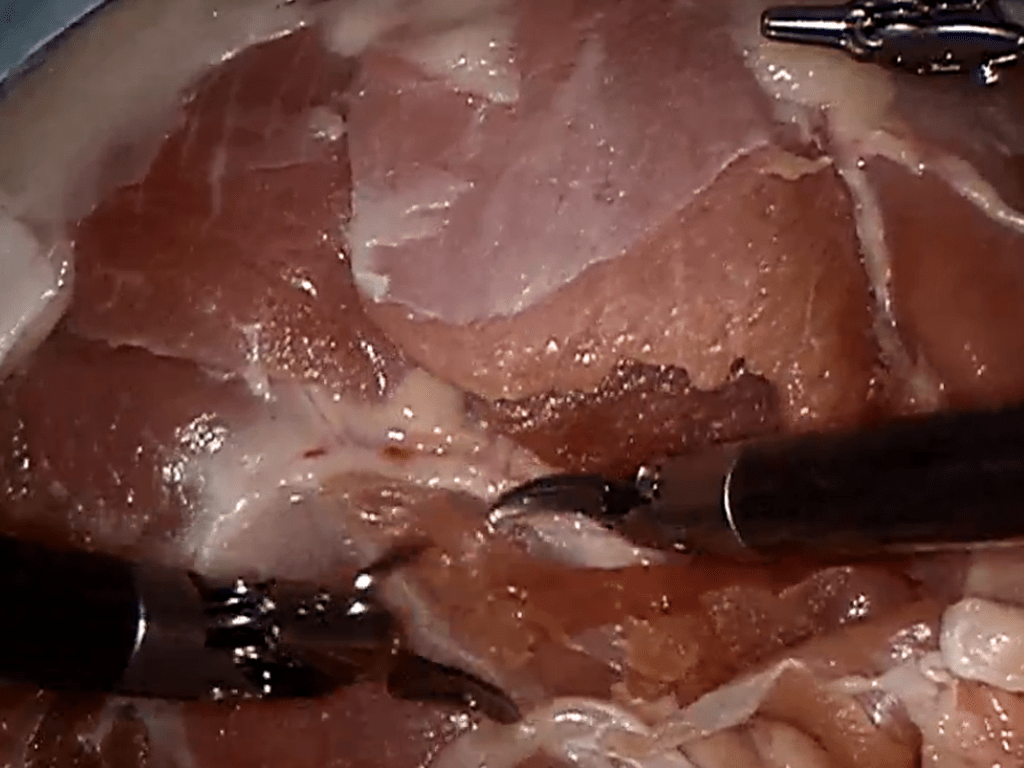
Reduction in Surgical Site Infections (SSI)
Clinical Initiatives to reduce Surgical Site Infections – Children’s Hospital desire to improve outcomes and reduce medical errors
Case Study Details
60% reduction in SSI
- 0.018% fewer SSI/admission
- 520 Bed Days Saved (time previously occupied by patients with SSI)
- 118 additional patients can be supported with the savings
Interventions aimed at reducing SSI rates were developed from published best practices and the institution’s internal observations and thoughts
- Developed process and procedures built around evidence based best practices, teamwork, and communications
- Used simulation to provide deliberate practice of these skills in simulated high risk, time pressured critical environments
- IRB granted exempt status, obtained confidentiality and video consent from all participants
- Participants required to participate in simulation but were not required to complete aptitude or knowledge surveys
2 days of non-clinical duty for each learner
- additional faculty time to develop curriculum
- additional cost to support simulation training for staff
< 1 year (2007)
Clinical resources to review best practices literature and adjust for internal constraints
- space to conduct simulation training
- properly trained faculty to support training initiative
- learner time to train away from clinical duties
Surgical Site Infection Rate on par with national average (1 per 100 surguries)
- based off of a 450 bed hospital
- based off of an admission rate of 28,000 per year
- 30% of admissions had surguries
- 1% of surguries had Surgical Site Infections
- Unnecessarily put at risk 50 patients per year
- prevent 118 patients to be cared for with the resources currently being used to treat patients with SSI
- within the US, potentially those costs must be absorbed by the institution since these are HAI, ~ $3.46 million/year
- loss of additional revenue from the 118 prospective patients, ~ $4.08 million/year
- net cost due to SSI if nothing is done ~ $7.54 million/year
Decision Maker Talking Points
- Unnecessarily put at risk 50 patients per year
- prevent 118 patients to be cared for with the resources currently being used to treat patients with SSI
- net cost due to SSI if nothing is done ~ $7.54 million/year
- If we implement program, for community PR show advocacy for Patient Safety, blowing past national average
- can be part of any number of patient safety movements, also good for PR
- Unnecessarily put at risk 50 patients per year
- risk of potential liability cost if publically know, preventable SSI
- potential liability of ~7.54 million/year
- cost of learners is 2 days of simulation and training/year
- training can be merged with VAP reduction
- Unnecessarily put at risk 50 patients per year
- prevent 118 patients to be cared for with the resources currently being used to treat patients with SSI
- If we implement program, for community PR show advocacy for Patient Safety, blowing past national average
- can be part of any number of patient safety movements, also good for PR
- training can be merged with VAP reduction
- need to train medical students with evidence based best practices
- need to have medical students training in an IPE environment to best prepare for current needs in Hospitals
- have students prepared to operate in high risk, time pressured critical environments
- better preparing the medical students given limitations on clinical hours
- practicing in a simulated environment instead of on actual patients
- need to train nursing students with evidence based best practices
- need to have nursing students training in an IPE environment to best prepare for current needs in Hospitals
- have students prepared to operate in high risk, time pressured critical environments
- better preparing the nursing students given limitations access to clinical placements
- practicing in a simulated environment instead of on actual patients
- Unnecessarily put at risk 50 patients per year
- ability to retain staffing by showing value for patient safety
- higher retention of learning through deliberate practice in team environments
- ability to better adjust behavior as teams train together
- training can be merged with VAP reduction
- making the case will involve a fully engaged staff of passionate educators
- make clear that faculty educators must be trained to conduct deliberate practice and feedback
- support a part of the institutions patient safey initiative to align with mission focus
- focus on capturing the appropriate ROI metrics for you environment
- training can be merged with VAP reduction
