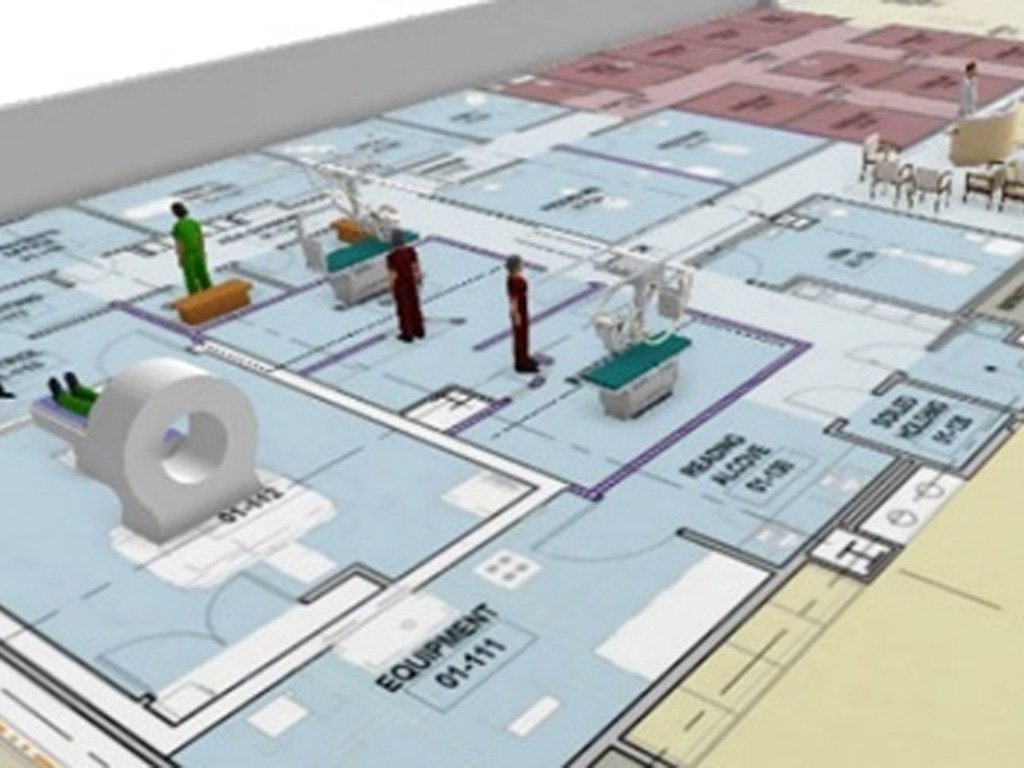
Simulating before Opening to Assess New Facilities
Using simulation, our objective was to define optimal staff roles, refine scope of practice, and identify LSTs before opening a new satellite hospital pedeatric ED
Case Study Details
Identified 37 LST focused around Equipment and Resources
Identified 46 errors in clinical proficiencies
- Laboratory simulations were used to define roles and scope of practice
- After each simulation, teams were debriefed using video recordings
- Simulations were scored for team behaviors by video reviewers using the Mayo High Performance Team Scale
- Subsequent in situ simulations focused on identifying LSTs and monitoring for unintended consequences from changes made
- ₤74,250 per annum
- ₤46,800 Staff Training
- ₤17,450 Protected Training Time
- ₤10,000 Consumables/Simulator
3 months
- prior to opening
81 Health care providers participated
- Nurses
- Paramedics
- Physicians
New Facility, no baseline data for performance
- done to identify Latent Safety Threats
- The 37 LST would have had patient safey implications
- The 46 clinical proficiency errors would have had patient safety implications
Decision Maker Talking Points
- Identified 37 LST focused around Equipment and Resources
- Identified 46 errors in clinical proficiencies
- Harm would have come to patients if this had not been done
- potentially damaging new hospital and ED reputation
- Identified 37 LST focused around Equipment and Resources
- Identified 46 errors in clinical proficiencies
- potentially damaging new hospital and ED reputation
- Identified 37 LST focused around Equipment and Resources
- Identified 46 errors in clinical proficiencies
- potentially damaging new hospital and ED reputation
- need to train medical students with evidence based best practices
- need to have medical students training in an IPE environment to best prepare for current needs in Hospitals
- have students prepared to operate in high risk, time pressured critical environments
- better preparing the medical students given limitations on clinical hours
- practicing in a simulated environment instead of on actual patients
- need to train nursing students with evidence based best practices
- need to have nursing students training in an IPE environment to best prepare for current needs in Hospitals
- better preparing the nursing students given limitations access to clinical placements
- practicing in a simulated environment instead of on actual patients
- Teams need to be assessed in simulation and not on patients
- better informed about staff to properly structure team education as needed
- ability to retain staffing by showing value for patient satisfaction
- ability to better adjust behavior as teams train together
- making the case will involve a fully engaged staff of passionate educators
- make clear that faculty educators must be trained to conduct deliberate practice and feedback
- support a part of the institutions patient safey initiative to align with mission focus
- focus on capturing the appropriate ROI metrics for you environment
